Mental health dietitians can help people to eat well and develop a positive relationship with food. Good nutrition is important for both your mental and physical health. Mental health dietitians also work to improve catering and menu planning within mental health settings, such as psychiatric units.
In this latest blog, Lauren Fisher, a recently registered dietitian at Oxford Health NHS Foundation Trust, reflects on her time in inpatient mental health settings, the challenges, the rewards, and learnings from her experience as a mental health dietician nine months into her role.
A day in the life of a band 5 mental health dietitian
Since starting at OHFT in July 2022, I have been covering the seven general adult and older adult inpatient mental health wards. My caseload includes nutrition support, weight management, refeeding syndrome, type 2 diabetes, dysphagia, coeliac disease, and disordered eating. While there are a wide range of nutritional needs among mental health patients, I am never the sole intervention in a patient’s journey within mental health services and the nutritional intervention will be provided in adjunct to the treatment for their mental health condition. Multidisciplinary team working is vital.
In addition to this, I also spend time working with the ward and catering teams to support patients with food allergies and other special dietary requirements. Through working alongside our Food Services Dietitian, I have gained a greater appreciation for the role of dietitians in advocating for high quality food services and the importance of the food service in fostering good nutrition practices. While most of my time is spent working clinically, some time is also spent focusing on projects, delivering staff training, developing resources, supporting our new Dietetic Apprentice and students, undertaking the preceptorship programme, and continuing to establish our dietetic service.
Going back to basics
Much to my surprise, there was not a permanent dietetic service for the inpatient mental health wards prior to my post. I was lucky to be starting from scratch with the help of my line manager, to develop the service into something we wanted it to be. This even meant putting together referral criteria! Before long, I was receiving an influx of referrals and it was clear that the ward teams saw value in the role of the Dietitian in patient care.
One of my first projects was a Nutrition Screening Audit, with the view to assess compliance with and the quality of nutrition screening on the wards and to identify dietetic needs from this. A brief outline of the project is below:
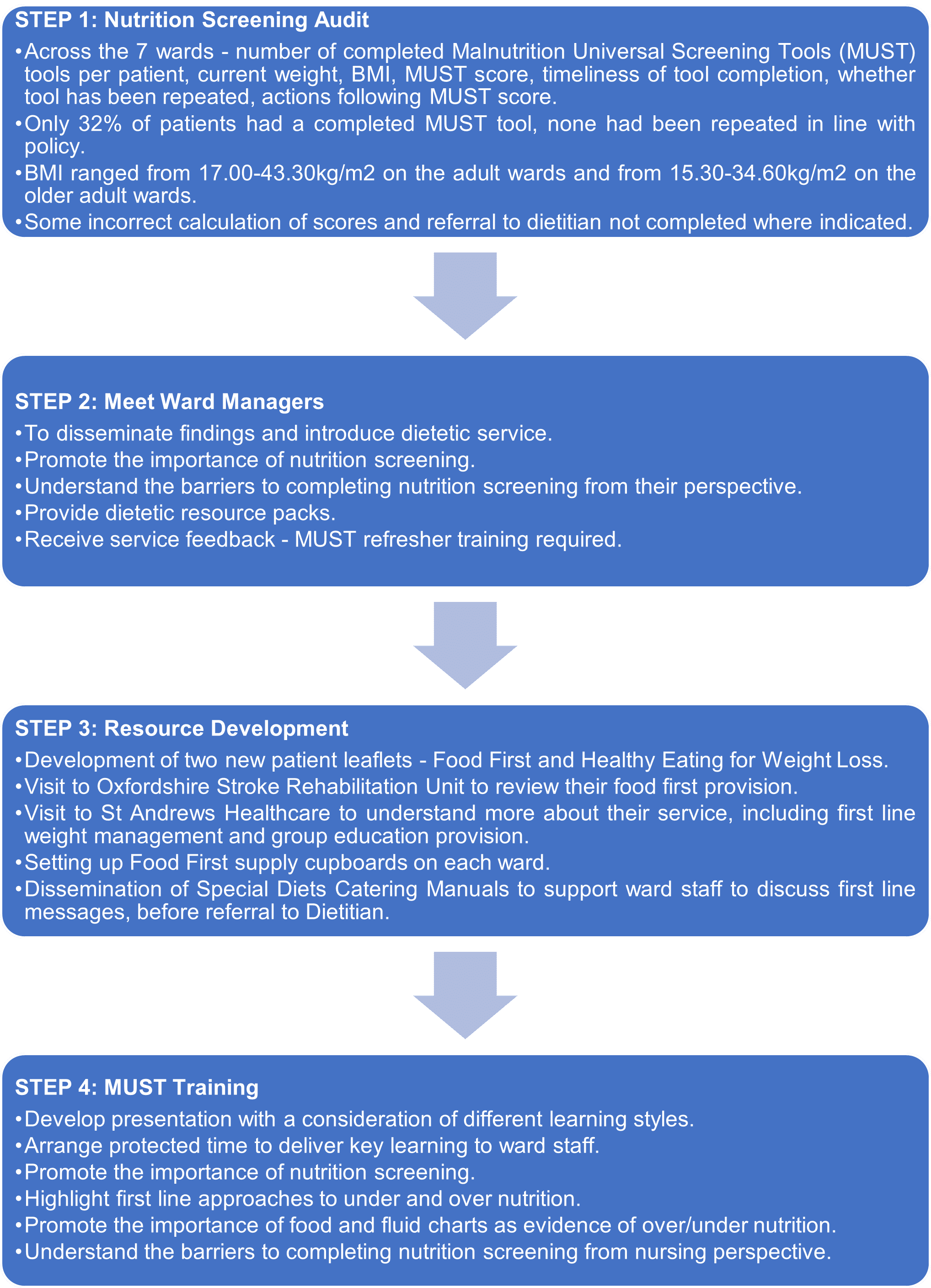
Figure 1: Step-by-step overview of the nutrition screening project.
The MUST training sessions took the form of a two-way conversation, and the focus was to disseminate key dietetic messages and understand the challenges with nutrition screening and monitoring at a ward levelFor example, one ward commented that there was a lot of paperwork (such as food and fluid, bowels, urine output, blood glucose) and they wanted to look at condensing this onto one form. They started a quality improvement project to trial this and I liaised with the project lead to help ensure that the ‘food and fluid’ section remains comprehensive to aid accurate dietetic assessment.
Professional development
As a newly qualified clinician at OHFT, I can undertake a year of preceptorship to develop my skills and confidence as an autonomous practitioner. Once a month, we meet to partake in workshops covering topics such as accountability, leadership within the NHS, inclusive communication, and patient safety. It is a great opportunity to network, share ideas and feel a sense of belonging within the Trust.
Early on in my role, I was also fortunate to attend the Introduction to Mental Health, Learning Disability and Eating Disorders course run by the British Dietetic Association. I was grateful to learn how fundamental dietetic skills are transferrable to the mental health setting. Another key take home message was around effective practice and ensuring that dietetic care is provided to as many people as possible and those who will benefit the most. Given this and the need for weight management intervention on the wards, I instigated work to set up Healthy Eating Groups, which our Dietetic Apprentice and Physio Technical Instructor are due to launch in the coming weeks.
Involvement in training the future workforce
Student training was an aspect of the job and since starting nine months ago, I have been involved in training Student Dietitians, our Dietetic Apprentice and Student Nurses. As newly qualified band 5 dietitians, we are well placed to be involved in student training, having been students not too long ago ourselves. I have particularly enjoyed encouraging students to reflect on their strengths each day and helping them to devise SMART goals and action plans for their next placement session. It is really rewarding to see students develop and achieve their goals. Recently, a Student Nurse also asked if she could shadow me for the morning to understand more about the role of the Dietitian. I would encourage other Dietitians to take up these opportunities, as they are a great way to promote the importance of nutrition to the new nursing workforce.
Take home messages
The last nine months have been a fantastic opportunity and I am grateful to have had experience in a specialism so early on in my career. This opportunity has developed my resilience to new challenges and I believe this stands me in good stead should I choose to work in other areas which are unfamiliar. I have particularly enjoyed the involvement in developing a dietetic service and the fact that every day is different
Working in inpatient mental health can be quite emotionally demanding, as we see our patients at their most unwell and vulnerable. However, this role has shown me that small changes and working in a kind and compassionate way can bring so much value to a patient’s journey. It is a privilege to feel that you can be part of this journey and improve one aspect of their health, even when things are incredibly tough for them.
I would encourage all band 5 dietitians with an opportunity to work in mental health to give it a go and put their core dietetic skills to practice in such a rewarding environment. Similarly, I would encourage Dietetic Leads within mental health services to consider opportunities for student training, workforce expansion and the development of roles for new graduates.